Published
Profession
Industry
Seniority
Published
Profession
Industry
Seniority
0
jobs
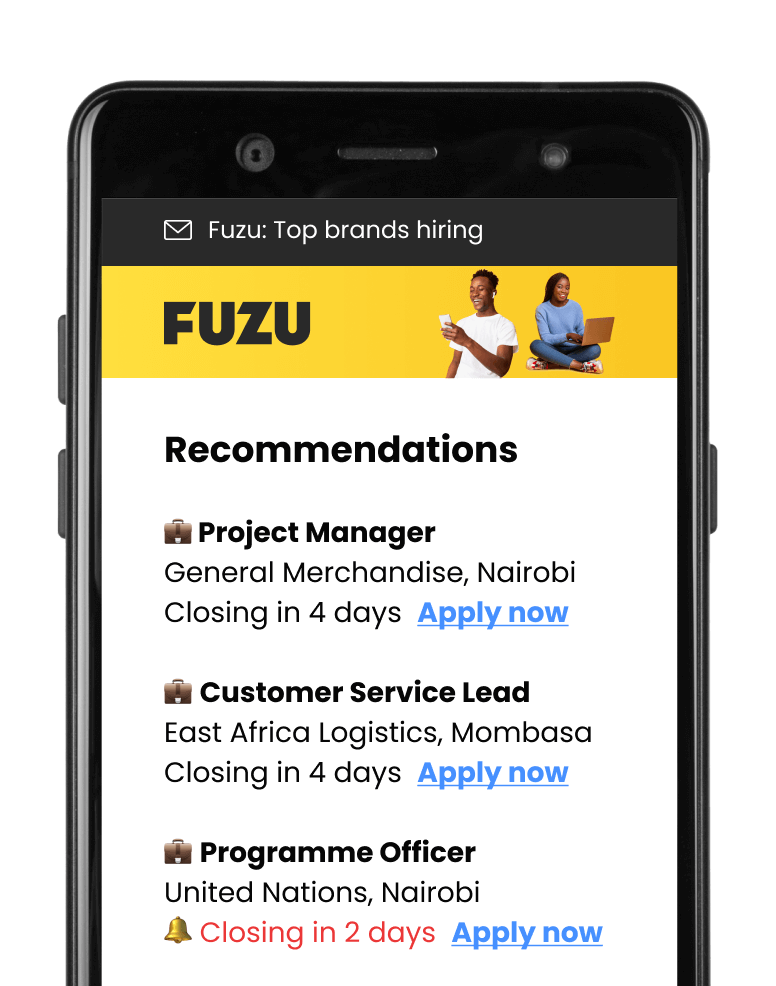
Get personalised job alerts directly to your inbox!
Reliance Health
CLOSEDLagos, Nigeria
Closing: Apr 5, 2024
This position has expiredPublished: Mar 27, 2024 (22 days ago)
Education:
Work experience:
Language skills:
Contract Type:
Sign up to view job details.
Applications submitted via Fuzu have 32% higher chance of getting shortlisted.