Published
Last 1 week
Last 30 days
Latest 24 hours
Industry
Health care, medical jobs
Seniority
Published
Profession
Industry
Seniority
0
jobs
Penda Health
CLOSEDNairobi, Kenya
Imara Mediplus Hospital
CLOSEDEmbu, Kenya
Uganda Non Communicable Diseases Alliance (UNCDA)
CLOSEDKampala, Uganda
eHealth4everyone
CLOSEDAbuja, Nigeria
eHealth4everyone
CLOSEDLagos, Nigeria
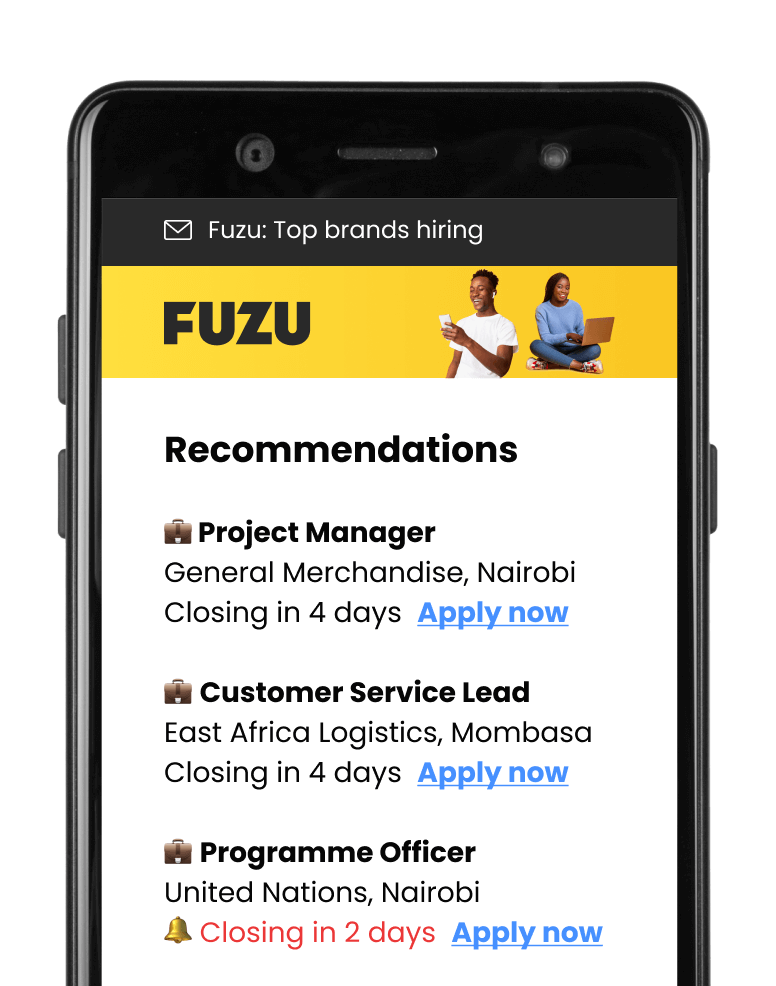
Get personalised job alerts directly to your inbox!
Lily Hospitals
CLOSEDLagos, Nigeria
Closing: May 2, 2024
This position has expiredPublished: Apr 29, 2024 (7 days ago)
Education:
Work experience:
Language skills:
Contract Type:
Sign up to view job details.
Key requirements and attributes
Key requirements and attributes
Applications submitted via Fuzu have 32% higher chance of getting shortlisted.