Published
Last 1 week
Last 30 days
Latest 24 hours
Profession
Industry
Published
Profession
Industry
Seniority
61
jobs
African Management Institute
Nairobi, Kenya
Save the Children (Kenya)
Nairobi, Kenya
KCB Group
Nairobi, Kenya
Norwegian Refugee Council
Nairobi, Kenya
KCB Group
Nairobi, Kenya
CARE International
Nairobi, Kenya
Majorel Kenya Limited
Mombasa, Kenya
Kenya Marine and Fisheries Research Institute
Mombasa, Kenya
One Acre Fund
Nairobi, Kenya
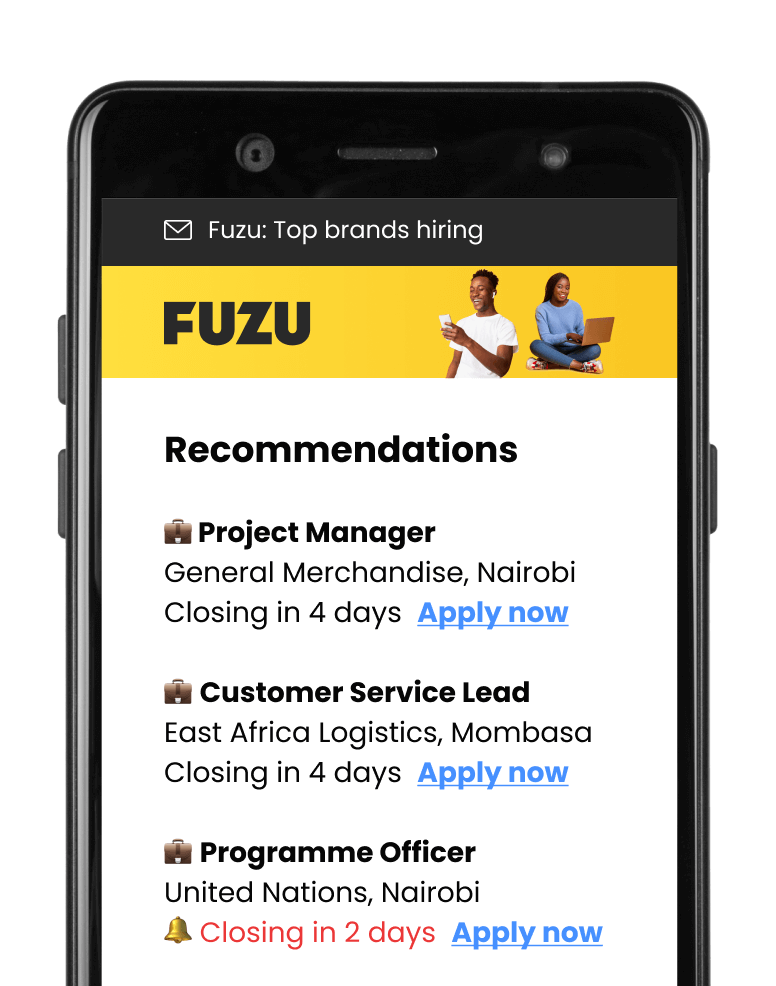
Get personalised job alerts directly to your inbox!
Ufanisi Digital Media
Only on FuzuNairobi, Kenya
Closing: Apr 24, 2024
5 days remainingPublished: Mar 29, 2024 (22 days ago)
Education:
Work experience:
Language skills:
Contract Type:
Sign up to view job details.
We are seeking a highly skilled and experienced Data Analyst to support our SME programs. The Data Analyst will be responsible for configuring and analyzing enterprise-level data and core SME metrics for program graduates. The Data Analyst will work closely with the Product Operations Manager, M&E team, Senior Data Engineer and Data Visualization Specialist to ensure that data is accurately captured, cleaned, validated, and analyzed to support decision-making and program improvements.This role is critical for data management, including solid processes to capture, clean, validate, and analyze key financial metrics.
This is a chance for an outstanding learning data practitioner to be part of Africa’s transformation, and to help shape, build and scale one its most innovative social businesses.
Requirements
Qualifications & Experience
BenefitsWhy join us
A dynamic office & team life:
We are seeking a highly skilled and experienced Data Analyst to support our SME programs. The Data Analyst will be responsible for configuring and analyzing enterprise-level data and core SME metrics for program graduates. The Data Analyst will work closely with the Product Operations Manager, M&E team, Senior Data Engineer and Data Visualization Specialist to ensure that data is accurately captured, cleaned, validated, and analyzed to support decision-making and program improvements.This role is critical for data management, including solid processes to capture, clean, validate, and analyze key financial metrics.
This is a chance for an outstanding learning data practitioner to be part of Africa’s transformation, and to help shape, build and scale one its most innovative social businesses.
Requirements
Qualifications & Experience
BenefitsWhy join us
A dynamic office & team life:
Applications submitted via Fuzu have 32% higher chance of getting shortlisted.