The suitable candidate should.
*Prove working experience as HR Manager or other HR Executive
*People oriented and results driven
*Demonstrable experience with Human Resources metrics
*Knowledge of HR systems and databases
*Ability to architect strategy along with leadership skills
*Excellent active listening, negotiation and presentation skills
*Competence to build and effectively manage interpersonal relationships at all levels of the company
*In-depth knowledge of labor law and HR best practices
Reporting to the Head of Human Capital
• Maintaining and enhancing the organization's human resources functions,
• Ensuring the effective implementation of Company Policy, Human resource policies and Health and safety requirements,
• Ensuring Legal Compliance, Liaoning with the external agencies, Handling the legal matters and statutory requirements,
• Recruitments and Training, Handling the Union matters and CBA, Effective monitoring of the Performance appraisals, Monitoring the Time and attendance systems and HRMS, Handling the Employees Grievances and Disciplinary issues,
• Ensuring the Safety and Security of the company property-Internally and Externally, Enhancing the Employees engagement and Top-Bottom, Bottom-Top communications, Strive for Culture building as per the Company Vision, Mission and Values,
• Creating the alignment towards company goals and objectives and ensuring that departmental goals of Production, Quality, Wastages and Costs are being achieved.
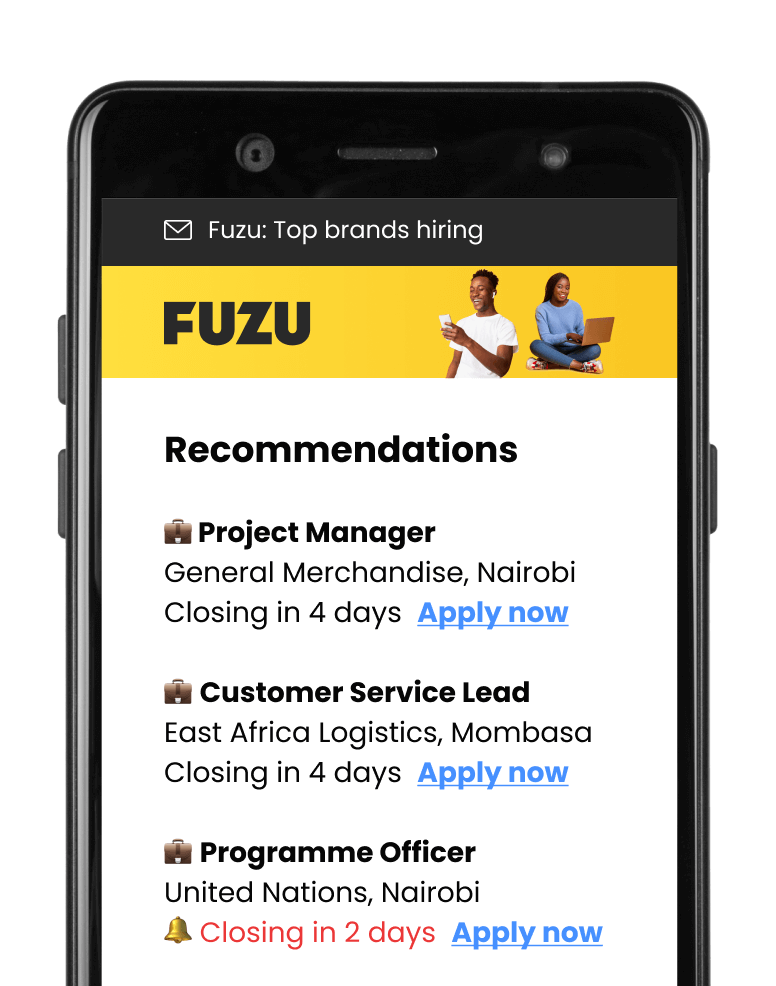
 Fast Apply
Fast Apply